If you've ever looked at a medical bill and wondered about all the leftover costs—the deductibles, the coinsurance, the copays—you're not alone. That's where a Medicare Supplement Plan, or Medigap, comes in. Think of it as a safety net for your Original Medicare.
It's not a replacement for Medicare. Instead, it's a separate policy you buy from a private insurance company. Its one job? To help cover the "gaps" in costs that Original Medicare (Part A and Part B) leaves behind. This makes your healthcare expenses far more predictable and manageable.
So, How Does a Medicare Supplement Plan Actually Work?
A Medigap plan partners with your Original Medicare. It doesn’t take over; it just fills in the financial holes. Imagine Original Medicare as your primary shield, deflecting the biggest healthcare costs. A Medigap policy is the second, smaller shield that steps in to block the costs that sneak past the first one.
The process is pretty seamless:
- You visit a doctor or hospital that takes Medicare.
- Medicare pays its approved share of the bill.
- Your Medigap plan then pays its portion, which might be your coinsurance, deductible, or copayment, depending on which plan you have.
This one-two punch is what helps keep your out-of-pocket costs down, giving you a powerful layer of financial protection. It's a system that over 14 million Americans rely on, and the market shows it. The U.S. Medicare Supplement market was valued at USD 28.53 billion in 2024 and is expected to hit USD 44.65 billion by 2033. That kind of growth is built on trust.
The Real Goal of a Medigap Plan
At its core, a Medigap plan is all about giving you peace of mind. It turns unpredictable medical bills into a steady, budget-friendly expense. Without one, you're on the hook for whatever Original Medicare doesn't cover, and there's no yearly cap on your out-of-pocket spending. That’s a scary thought for anyone on a fixed income.
A huge plus for Medigap is freedom. You can see any doctor, specialist, or hospital in the U.S. that accepts Medicare. No referrals needed. This flexibility is one of the biggest reasons people choose this path.
To really see where a Medigap plan shines, it helps to know what Original Medicare covers first. For example, understanding things like whether electric wheelchairs are covered by Medicare gives you a clearer picture of the gaps that need filling. For a deeper dive into all your options, our complete Medicare planning guide is a great place to start.
This visual helps show how everything fits together.
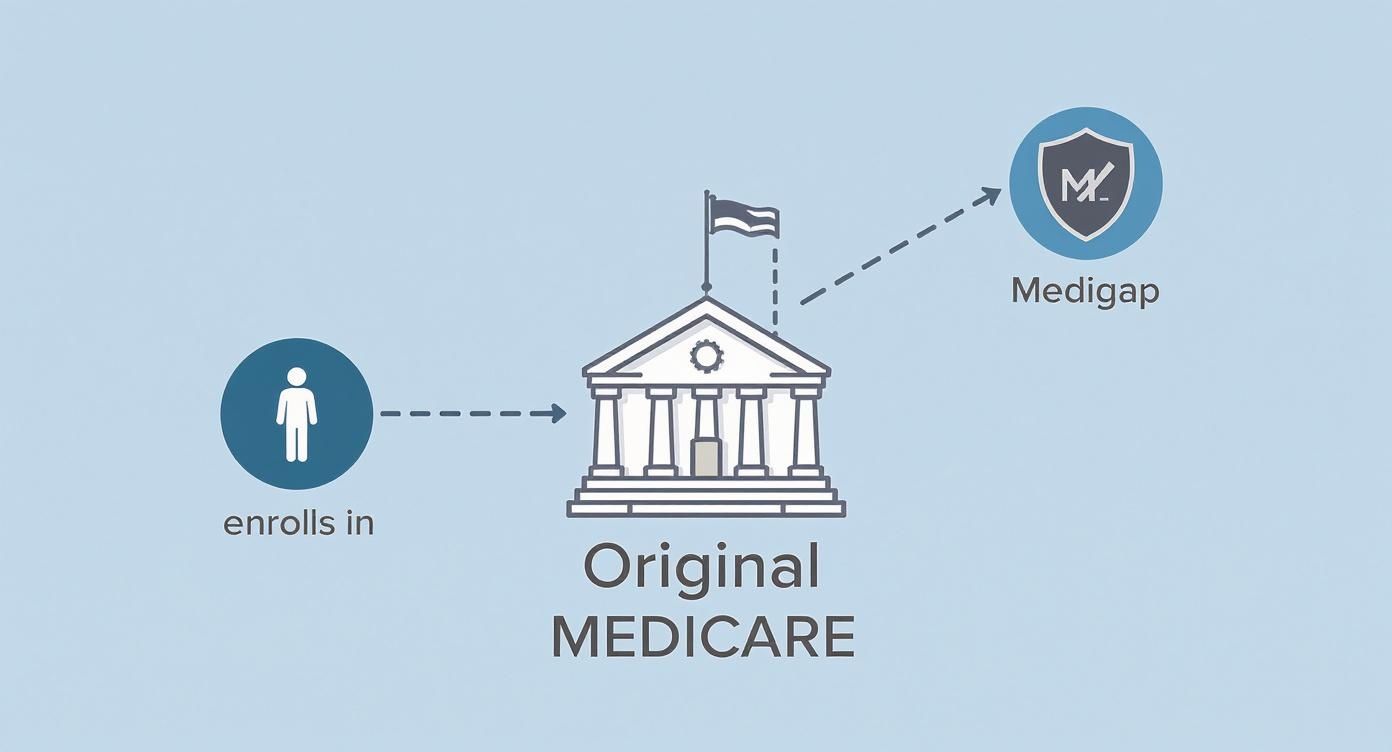
It’s a simple partnership: Original Medicare pays first, and your Medigap policy steps in to help with the rest.
Original Medicare vs. Medicare Supplement Coverage at a Glance
To make it even clearer, let's break down who pays for what. This table shows the costs Original Medicare typically handles versus the costs a Medigap plan is designed to cover.
| Cost Type | Covered by Original Medicare (Parts A & B) | Covered by Medicare Supplement (Medigap) Plans |
|---|---|---|
| Hospital Stays (Part A) | A large portion after you meet your deductible | Your Part A deductible, coinsurance, and potentially extended stays |
| Doctor Visits (Part B) | 80% of Medicare-approved costs after your deductible | Your 20% Part B coinsurance and potentially the deductible |
| Part A Deductible | No | Yes, on most plans |
| Part B Deductible | No | Yes, on some plans (for those eligible before 2020) |
| Skilled Nursing Coinsurance | No | Yes, on all current plans |
| Care Outside the U.S. | No | Yes, on several plans (up to plan limits) |
| Prescription Drugs (Part D) | No (this is separate) | No (you need a separate Part D plan) |
As you can see, a Medigap policy is specifically built to pick up the common out-of-pocket costs that can quickly add up under Original Medicare alone.
How to Read the Medigap Plan Letters
Navigating the world of Medigap plans can feel like trying to solve an alphabet soup puzzle. With plans labeled A, B, C, D, F, G, K, L, M, and N, it's easy to get overwhelmed. But there's one simple rule that cuts through all the noise: Medigap plans are standardized by the federal government.
This is a huge advantage for you. It means that a Plan G from one insurance company has to offer the exact same core benefits as a Plan G from another company. The only real differences you’ll find are the monthly premium and the company's customer service reputation.
That simple fact strips away the marketing hype. Instead of trying to compare confusing benefit packages, you get to compare apples to apples. Your decision boils down to price and service.
The Most Popular Plans: G, F, and N
While there are ten different plan options in most states, the truth is, most people end up choosing from just three: Plan G, Plan F, and Plan N. Get to know these three, and you'll have a solid grip on the entire Medigap landscape.
The numbers don't lie. Plan G is the clear favorite, with about 7.5 million people enrolled, making up roughly 55% of all Medigap policyholders. Plan F is next in line at 36%, followed by Plan N at 10%. These three plans dominate the market for a reason. You can discover more insights about Medigap enrollment trends to see just how popular they are.
Let’s dig into why these three are the go-to choices.
Plan G: The New Gold Standard
For anyone who became eligible for Medicare on or after January 1, 2020, Plan G is the most comprehensive coverage you can buy. It's often called the "new gold standard" because it plugs almost every single gap left by Original Medicare.
Here’s a quick look at what Plan G takes care of:
- Part A Coinsurance & Hospital Costs: Covers you for an extra 365 days after your Medicare benefits run out.
- Part B Coinsurance or Copayment: Pays the 20% that Medicare doesn't.
- First Three Pints of Blood: Covers the cost if you need a transfusion.
- Part A Hospice Care Coinsurance: Handles your share of hospice costs.
- Skilled Nursing Facility Care Coinsurance: Takes care of the daily coinsurance for skilled nursing care.
- Part A Deductible: This is a big one. Plan G covers this major hospital cost completely.
- Part B Excess Charges: Protects you if a doctor charges more than the Medicare-approved amount.
- Foreign Travel Emergency: Covers 80% of emergency care when you're traveling abroad, up to the plan's limit.
The only thing Plan G doesn't cover is the annual Medicare Part B deductible. Once you pay that small, once-a-year amount yourself, your Plan G kicks in and pays 100% of your Medicare-approved costs for the rest of the year.
Plan F: The Original All-in-One Plan
For years, Plan F was known as the plan with the most complete coverage you could get. It covers everything Plan G does, and it also pays for your annual Part B deductible. However, a change in federal law means Plan F is no longer available to people new to Medicare as of January 1, 2020.
Who can still buy Plan F? If you were eligible for Medicare before January 1, 2020, you might still be able to buy a Plan F. That said, many people find that Plan G offers better long-term value.
Because no new, younger members can join Plan F, its group of policyholders is getting older. This can lead to higher premium increases over time compared to Plan G.
Plan N: A Lower Premium Option with a Trade-Off
Plan N is a fantastic choice if you want solid protection but are okay with some small, predictable costs in exchange for a lower monthly premium. It covers most of the same big-ticket items as Plan G, but with a few key differences in how you share costs.
With a Plan N, you agree to pay:
- A copay of up to $20 for some doctor's office visits.
- A copay of up to $50 for a trip to the emergency room (this is waived if you're admitted to the hospital).
- The annual Part B deductible (just like Plan G).
- Potential Part B excess charges (Plan N does not cover these).
For many healthy, active people, the savings on the monthly premium make the occasional copay a smart trade-off. You still get robust protection from major medical bills while keeping your fixed monthly costs down.
Comparing the Top 3 Medigap Plans: G, F, and N
To make it even clearer, here's a side-by-side look at how the big three stack up. This table breaks down what each plan covers, so you can see the differences at a glance.
| Benefit | Plan G Coverage | Plan F Coverage (Only for those eligible before 2020) | Plan N Coverage |
|---|---|---|---|
| Part A Coinsurance | ✅ Yes | ✅ Yes | ✅ Yes |
| Part B Coinsurance | ✅ Yes | ✅ Yes | ✅ Yes (with small copays) |
| Blood (First 3 Pints) | ✅ Yes | ✅ Yes | ✅ Yes |
| Part A Hospice | ✅ Yes | ✅ Yes | ✅ Yes |
| Skilled Nursing Coinsurance | ✅ Yes | ✅ Yes | ✅ Yes |
| Part A Deductible | ✅ Yes | ✅ Yes | ✅ Yes |
| Part B Deductible | ❌ No | ✅ Yes | ❌ No |
| Part B Excess Charges | ✅ Yes | ✅ Yes | ❌ No |
| Foreign Travel Emergency | ✅ Yes (80%) | ✅ Yes (80%) | ✅ Yes (80%) |
As you can see, the differences are small but important. Plan F offers first-dollar coverage, Plan G covers almost everything except one deductible, and Plan N lowers your premium by adding a few copays. Choosing the right one comes down to your budget and how you prefer to pay for your care.
Choosing Between Medigap and Medicare Advantage
When you first sign up for Medicare, you’ll find yourself at a major fork in the road. One path leads to Original Medicare paired with a Medigap plan. The other path takes you to a Medicare Advantage (Part C) plan. Getting a real handle on how these two options work is the key to picking the right coverage for your life and your health.
Think of it like this: Medigap is the "Freedom of Choice" road. It works hand-in-hand with your Original Medicare, giving you the liberty to see any doctor or hospital in the entire country that accepts Medicare. No networks. No referrals to see a specialist. This path is all about flexibility and nationwide access.
The other road is Medicare Advantage, which is more of a "Managed Care" highway. These are all-in-one plans from private insurance companies that bundle your hospital (Part A), medical (Part B), and usually prescription drug (Part D) coverage together. They almost always operate within local networks, like an HMO or PPO, and you may need a referral to see a specialist.
Provider Access: The Core Difference
The single biggest distinction between these two choices is how you get your healthcare.
With a Medigap plan, your network is the entire country. If a doctor takes Medicare, they take your plan. Simple as that. This is perfect for people who travel a lot, live in different states part-time, or just want the peace of mind that comes with being able to see any specialist they choose.
Medicare Advantage plans, on the other hand, require you to use doctors and hospitals within their specific network to keep your costs down. If you go out-of-network, you could face much higher bills or even have no coverage at all, unless it's a true emergency. These networks can be great, but they are geographically limited, which can be a real problem if you need care while you're away from home.
The decision often comes down to a simple trade-off: Would you prefer paying a higher monthly premium for the freedom to see any provider (Medigap), or a lower (sometimes $0) premium in exchange for staying within a local provider network (Medicare Advantage)?
Comparing Costs and Coverage
The way you pay for care is also completely different.
With a Medigap plan, you pay a set monthly premium to your insurance company. In return, that plan covers most—or all—of your out-of-pocket costs like coinsurance and deductibles. This leads to very predictable, stable healthcare spending. You will, however, need to buy a separate Part D plan for your prescriptions.
Medicare Advantage plans often look attractive with their low or even $0 monthly premiums. But you’ll pay for services as you use them through copayments and coinsurance. While these plans have a yearly maximum out-of-pocket limit, your costs can swing wildly depending on how much medical care you need. On the plus side, many Advantage plans include extra benefits not covered by Original Medicare, like routine dental, vision, and hearing services.
Making the Right Choice for You
There's no single "best" answer here. The right choice is deeply personal and depends entirely on your priorities.
A Medigap plan might be the better fit if you have ongoing health issues and want predictable costs and total freedom to choose your doctors. An Advantage plan could be a great option if you're healthy, don't mind staying in a network, and want an all-in-one plan with a low premium and extra perks.
It's also critical to know that switching between these plans isn't always easy. While you can usually move from Medigap to Advantage, going the other way can be tough. If you decide to switch from Medicare Advantage to Medigap after your initial enrollment window, you might have to answer health questions and could be denied coverage. Thinking carefully about your options now can save you a world of trouble down the road.
When and How to Enroll in a Medigap Plan
When it comes to Medigap, timing is everything. Seriously. There’s one window of opportunity that’s more important than any other: your Medigap Open Enrollment Period.
This is a one-time, six-month period that kicks off the first day of the month you’re both 65 or older and signed up for Medicare Part B. Think of it as your golden ticket.
During these six months, you have what are called "guaranteed issue rights." This is a powerful protection. It means private insurance companies must sell you any Medigap policy they offer, no matter your health history. They can't charge you more or deny you coverage because of a pre-existing condition.
Miss this window, and you could face some tough hurdles down the road.
Why This Enrollment Period Is So Critical
Once your Medigap Open Enrollment Period closes, it’s gone for good. If you try to buy a plan later, insurers in most states can put you through full medical underwriting.
That means they’ll dig into your entire health history. And based on what they find, they can legally do a few things you won’t like:
- Charge you a higher monthly premium because of your health.
- Flat-out refuse to sell you a policy if they decide you’re too much of a risk.
It's like a protected harbor. Inside, every ship gets the same treatment. But once you sail out, you’re on the open seas, and your journey depends entirely on the weather—or in this case, your health. It’s the single most important deadline to know.
Special Situations and Guaranteed Issue Rights
So what happens if you miss that initial window? While the six-month period is your main shot, certain life events can trigger another chance to buy a Medigap plan with guaranteed issue rights.
These special rights usually pop up when you lose other health coverage through no fault of your own. For example, maybe your old employer plan is ending, or you’re moving and your Medicare Advantage plan won’t work in the new area.
Here are a few common situations that might open a new door for you:
- Losing Employer Coverage: You worked past 65 but are now leaving your job and its health plan.
- Moving: You have a Medicare Advantage plan and are moving somewhere your plan doesn’t cover.
- Plan Misconduct: Your insurance company misled you or broke the rules.
These protections are there so you aren't left stranded. Losing your job’s health insurance is a big deal, and it's crucial to understand what is creditable coverage to avoid late enrollment penalties. Getting these rules right keeps your options open and your costs down. Just remember to act fast—these special enrollment windows are short, often lasting only 63 days after your other coverage ends.
Understanding the Cost of a Medigap Plan
So, you've got the basics down on what a Medicare Supplement plan is. The next big question is usually, "Okay, but what's it going to cost me?"
There’s no simple price tag. The monthly premium for a Medigap plan isn’t a one-size-fits-all number. It’s shaped by a handful of key factors, and getting a handle on them is the secret to finding a plan that protects both your health and your wallet for years to come.
One of the biggest puzzle pieces is how an insurance company actually sets its prices over time. It’s not something most people think about, but it can make a huge difference in what you pay as you get older.
How Insurance Companies Rate Your Premium
Think of these "rating methods" as different roads your premium can travel down over the years. Some are slow and steady, while others have some steep hills ahead.
-
Community-Rated: This is often the most predictable path. Everyone in a certain area with the same plan pays the same premium, whether they're 65 or 85. Your rate will still creep up with inflation, but it won’t jump just because you celebrated another birthday.
-
Issue-Age-Rated: Here, your premium is locked in based on your age when you first buy the policy. If you sign up at 65, you'll have a lower rate for life than someone who signs up at 70. Again, your premium can still rise with inflation, but not because you're getting older.
-
Attained-Age-Rated: This is the most common model you'll see. The premium starts low, based on your current age, but it's designed to increase as you get older. Those increases can feel pretty sharp in your late 70s and 80s, which is why it's so important to think about the long game.
Understanding the rating method isn't just a minor detail—it's essential for your long-term budget. A plan that looks like a bargain at age 65 might feel unaffordable by age 80 if it's an attained-age plan. Always ask which method the insurer uses.
Other Factors That Influence Your Cost
Beyond how a company rates its policies, a few other things come into play when calculating your monthly premium.
The plan letter you choose is a huge one. A comprehensive plan like Plan G is naturally going to cost more than a plan with more cost-sharing, like Plan N. Where you live also makes a big difference—healthcare costs vary a lot by state and even zip code.
Some insurers offer household discounts if you and a spouse or partner enroll together. And lifestyle choices, especially tobacco use, will almost always mean a higher premium. To lock in the best rates, it’s a good idea to check out our guide on the best Medicare Supplement plan options out there.
Why the Insurance Company Matters
Here’s something that trips people up: Medigap plans are standardized by the government, but the companies selling them are not.
The Medigap market is led by a few big names. As of 2022, UnitedHealth Group had the largest slice of the pie at 31.7% market share. They were followed by Mutual of Omaha Group (9.9%) and CVS Group (Aetna) at 8.7%. Those three companies alone cover about half of all Medigap policyholders.
Because every company sets its own rates, the premium for the exact same plan can be wildly different from one insurer to the next. Company A might have a great rate on Plan G in your county, while Company B is the most competitive for Plan N.
This is why shopping around is the single most powerful thing you can do. Comparing quotes from several top-rated insurers is the only way to be sure you aren’t overpaying for your coverage.
Common Questions About Medicare Supplement Plans
Once you start to grasp how Medigap works, the real-world questions bubble up. The details can feel a little tangled, but getting straight answers is how you make a decision you can feel good about. This final section digs into the most common questions people have after they’ve learned the basics.
Let's clear up the confusion around switching plans, prescription drugs, and those extra benefits like dental and vision. Nailing down these points will help you know what to expect and plan your healthcare coverage with confidence.
Can I Switch My Medigap Plan Later On?
This is one of the biggest questions out there, and the honest answer is: it’s tricky. While you can technically apply for a different Medigap plan whenever you want, getting approved is a whole other ballgame.
Your golden ticket is your one-time, six-month Medigap Open Enrollment Period. During this window, you have "guaranteed issue rights." That’s a fancy way of saying insurance companies can't turn you down or charge you more because of your health. It’s your one free pass.
Once that period closes, those protections vanish in most states. If you decide you want to switch from a Plan N to a Plan G a few years later, you'll almost certainly have to go through medical underwriting.
This means the insurance company will put your health under a microscope, asking detailed questions and digging into your medical records. Based on what they find, they have the right to:
- Approve your application at their normal rate.
- Charge you a higher premium because of your health status.
- Deny your application flat-out.
Switching a Medigap plan isn't like changing your car insurance. After that initial window, your health becomes the single most important factor. This is exactly why picking the right plan from the very start is so critical.
There are a few exceptions, of course. Some states, like California and Oregon, have a "birthday rule" that gives you an annual window to switch plans. Big life events, like moving to a new state, can also trigger a special enrollment period with guaranteed issue rights. But for most people, that first six-month window is their best—and only—guaranteed shot.
Do Medigap Plans Cover Prescription Drugs?
This is a huge point of confusion, so let’s make it crystal clear: No, the standardized Medigap plans sold today do not include prescription drug coverage.
It's how the whole system was designed. Medigap plans exist to fill the gaps—the "holes"—in Original Medicare Part A (hospital) and Part B (medical). They’re built to handle costs like deductibles and coinsurance for your hospital stays and doctor visits.
Prescription drug coverage is a completely different piece of the puzzle: Medicare Part D.
To get your medications covered, you have to sign up for a separate, standalone Medicare Part D Prescription Drug Plan. It’s a policy you buy from a private insurer, and it comes with its own monthly premium. It works right alongside your Original Medicare and Medigap plan to give you a complete safety net.
Why the confusion? Some very old Medigap plans sold before 2006 did have some drug coverage, but federal law changed all that. Forgetting to sign up for Part D when you're first eligible can stick you with a late enrollment penalty that you'll pay for the rest of your life. It’s a step you can't afford to miss.
Does Medigap Cover Dental, Vision, or Hearing?
Another frequent question is whether Medigap will help pay for things like routine dental cleanings, a new pair of glasses, or hearing aids. The answer here is just as direct: No, standard Medigap plans do not cover routine dental, vision, or hearing services.
The reason is simple. Medigap only supplements costs for services that Original Medicare covers. Since Original Medicare doesn't cover these routine services in the first place, Medigap has nothing to "supplement."
If you need coverage for these essential services, you have a couple of solid options:
- Buy a separate, standalone insurance plan just for dental, vision, or hearing. Plenty of companies offer these policies.
- Look into a Medicare Advantage (Part C) plan instead. Many Advantage plans bundle these extra benefits into their all-in-one package. This is one of the key trade-offs to weigh when you're deciding which path to take.
It's all about managing expectations. A Medigap plan offers incredible financial protection against the major medical costs Medicare covers, but it was never meant to be an all-in-one health plan. You'll need to plan and budget for your medications and other care like dental, vision, and hearing separately.
Figuring out your Medicare options can feel like a maze, but you don't have to walk it alone. The experts at My Policy Quote are here to offer personalized guidance, helping you compare plans from top-rated carriers to find the perfect fit for your life and your budget. Visit us at https://mypolicyquote.com to get your free, no-obligation quotes today and take the first step toward a secure healthcare future.

