When Medicare denies a claim, it feels personal. It’s frustrating, confusing, and can leave you wondering what to do next. But a denial isn't the end of the road. It's the beginning of a conversation, and you have every right to challenge a decision you believe is wrong.
The Medicare appeals process is your official path to do just that. It's a structured system with five distinct levels, starting with a simple request and potentially escalating from there.
Decoding Your Medicare Claim Denial
That denial letter—your Medicare Summary Notice (MSN) or Explanation of Benefits (EOB)—is more than just bad news. It's a map. Before you can fight back effectively, you have to understand why the claim was denied in the first place. This is where you shift from feeling like a victim of the system to becoming your own best advocate.
Denials can happen for all sorts of reasons, from a simple typo to a major disagreement over what’s considered medically necessary.
Common Reasons for Medicare Denials
- Clerical Errors: You'd be surprised how often a misspelled name, a flipped digit in a policy number, or the wrong billing code is the culprit. These are usually the easiest fixes.
- Lack of Prior Authorization: Some treatments and services need a green light from Medicare before you receive them. If that didn't happen, a denial is almost automatic. The world of pre-approvals is complex, and even innovations like AI prior authorization can't prevent every hiccup.
- Not Medically Necessary: This one is tougher. It means Medicare has decided the service or supply wasn't essential for your condition based on their official guidelines.
- Insufficient Documentation: Your doctor or provider might not have sent enough detailed notes to justify the care. For example, if you're in physical therapy, but the therapist's notes don't clearly document your progress, Medicare might deny further sessions.
This visual breaks down the first three levels of the appeals process, giving you a clear sense of the timeline for each critical stage.
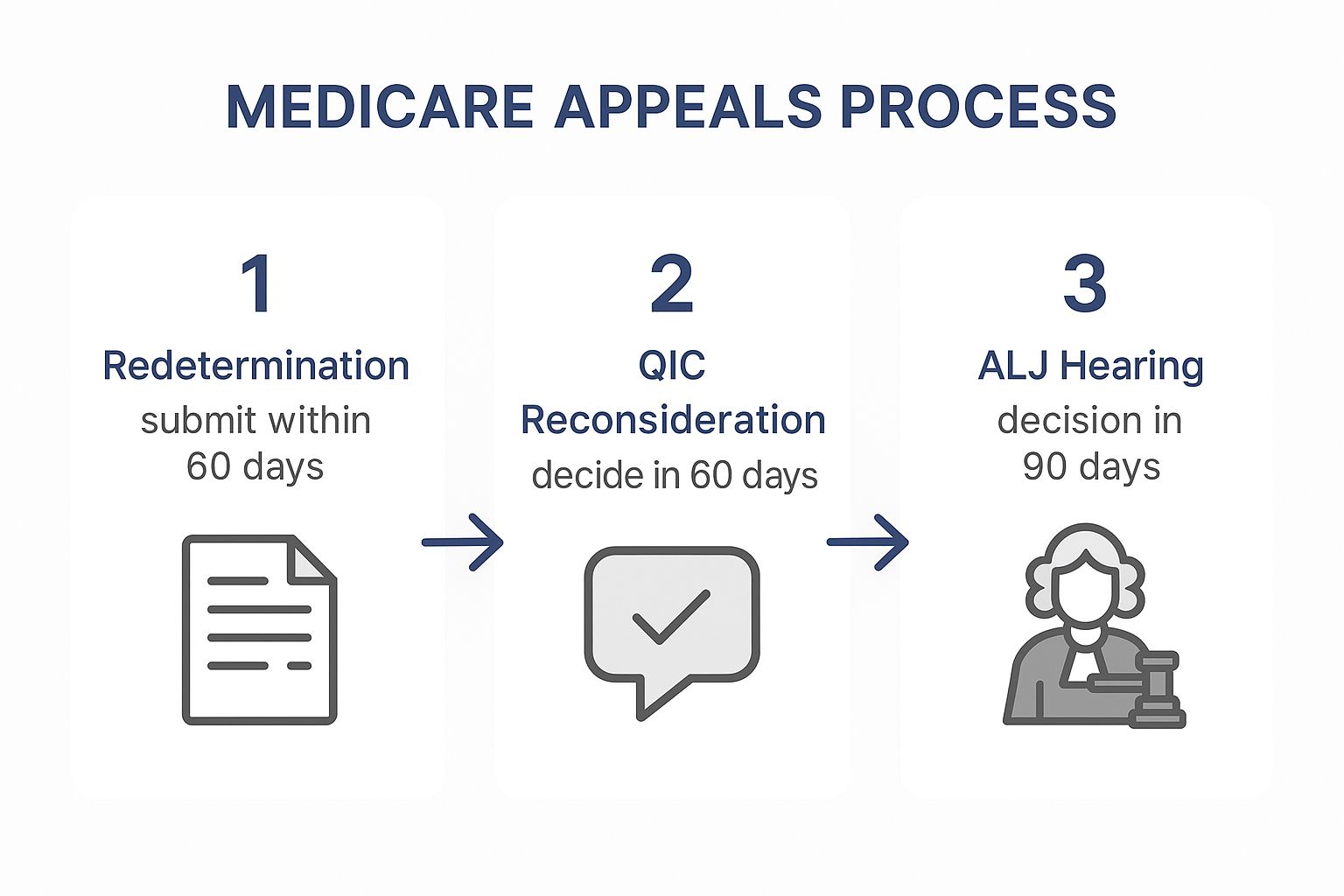
As you can see, each level has its own deadline. Acting quickly is key to keeping your appeal moving forward.
Why So Few People Appeal
Here’s a surprising fact: most people just give up. KFF data from 2023 shows that while a staggering 28.8% of prior authorization requests were denied, less than 7% of those denials were ever appealed.
But for those who do fight back, the odds can be pretty good. About 28.7% of first-level appeals are successful. That proves one thing: persistence pays off.
Your first step isn’t to argue—it’s to investigate. Call your provider’s billing office. A quick conversation can often reveal whether the issue was a simple coding error they can fix and resubmit on your behalf, saving you the trouble of a formal appeal.
Facing potentially high out-of-pocket costs is stressful, which is why having the right backup is so important. Looking into the best Medicare Supplement plan can provide a crucial safety net for the expenses Original Medicare won't cover, giving you peace of mind no matter what happens with a claim.
The First Two Levels: Where the Real Fight Begins
This is where your appeal journey gets serious. The first two stages are handled by Medicare contractors, and honestly, winning here comes down to two things: solid preparation and hitting your deadlines. Let's break down exactly what to do for Original Medicare claims, step by step.
The first round is called a Redetermination. Think of it as asking the same Medicare Administrative Contractor (MAC) that denied your claim to take a second look. You have a strict 120-day window from the date on your Medicare Summary Notice (MSN) to get this filed. If you miss that deadline, your appeal can be over before it even starts.
You'll need the "Medicare Redetermination Request Form" (Form CMS-20027) to get the ball rolling. On it, you’ll list the services being appealed and explain why the denial was wrong. Just saying "I disagree" won't cut it. You have to build a case.
Level 1: A Deeper Dive into Redetermination
The power of your Redetermination request lies in the evidence you submit. Don't just send the same old paperwork. You need to add new, compelling documents that directly challenge the reason for the denial.
- Your Doctor's Letter is Your Secret Weapon: Ask your doctor to write a detailed letter explaining why the service was medically necessary. This isn't just a prescription note; it should tell a story about your specific condition, your treatment history, and why this denied service is critical to your care.
- Back It Up with Medical Records: Attach copies of relevant office visit notes, lab results, or other records that support everything in your doctor's letter. Organize them neatly so the reviewer can easily connect the dots.
- Add Your Voice: A short, personal letter from you can be incredibly powerful. Explain how your condition impacts your daily life and why this treatment is so important for your health and well-being.
Once you’ve sent everything in, the MAC has 60 days to review your request and make a decision. A lot of simple mistakes get fixed here. But often, they stand by their original decision, which means it’s time to move on to the next level.
The CMS website has a page dedicated to the fee-for-service appeals process where you can find all the official forms and resources.

Bookmark that page. It’s your go-to for the latest forms and any procedural changes, ensuring you're always using the right documents.
Level 2: Reconsideration by a Fresh Pair of Eyes
If your Redetermination is denied, don't lose hope. You’ll get a letter explaining their reasoning, and now you can kick it up to the second level: Reconsideration. This time, your file goes to a Qualified Independent Contractor (QIC).
A QIC is a completely separate company hired by Medicare to provide a fair, unbiased review. They had nothing to do with the first denial, giving you a much better shot at an impartial decision. For this step, you get a 180-day window from the date of the Redetermination denial to file.
Pro Tip: That longer deadline is a gift. Use it wisely. Don't just rush to resubmit. Read the denial letter from Level 1 very carefully. It's your roadmap. Did they claim there wasn't enough evidence? Go get more. Did they misunderstand something? Clarify it.
For this level, you’ll fill out the "Medicare Reconsideration Request Form" (Form CMS-20033). Just like before, you need to clearly state your case, attach all your previous documents, and add any new evidence you've gathered. The QIC also has 60 days to decide. If they deny your appeal, your next stop is a hearing with an Administrative Law Judge.
Advancing Your Case To Higher Appeal Levels
It’s easy to feel defeated if your claim gets denied at the first two levels. But the fight isn’t over yet. The next stages of the Medicare appeals process shift into a more formal, court-like setting.
This is where a fresh set of eyes will look at your case from a legal perspective, and it’s where all your detailed preparation can really start to shine.
Your next stop is a hearing with an Administrative Law Judge (ALJ), who works for the Office of Medicare Hearings and Appeals (OMHA). This is a big deal. For the first time, you or your representative can actually present your case live to a judge. These hearings usually happen over video or phone, but sometimes in person.
To get to this stage, your appeal needs to meet a minimum "amount in controversy." For 2025, that threshold is $190. You can learn more about the specifics directly from the government's fee-for-service appeals process on CMS.gov.
Preparing For Your ALJ Hearing
Winning at this level comes down to organization and making a clear, compelling argument. The ALJ is an impartial judge, but they are also an employee of the Department of Health and Human Services. Your goal is to lay out such a logical, evidence-based case that approving your claim is the only reasonable outcome.
Think of it like a mini-trial. You’ll present your evidence and can even have witnesses, like your doctor, testify on your behalf. Because everything needs to be submitted beforehand, knowing how to write a legal brief can be a game-changer for presenting your side effectively.
Here’s how to get ready:
- Organize Your Evidence: Get every single document related to your case and put it in a clear, chronological file.
- Draft a Position Paper: Write up a summary of your argument, making sure to reference specific documents and evidence.
- Prep Your Witnesses: If your doctor is going to testify, go over the key points you need them to make about why your care was medically necessary.
The Final Stages Of The Medicare Appeals Process
What if the ALJ rules against you? There are still two final, highly legalistic levels left in the Medicare appeals process. At this point, it’s less about the medical details and more about the letter of the law.
The fourth level is a review by the Medicare Appeals Council. The Council, which is part of HHS, looks over the ALJ's decision. There's no live hearing here; they just review the written record and all the briefings to decide if the ALJ made the right legal call.
If the Appeals Council also denies your claim, the fifth and final step is a Judicial Review in a U.S. District Court. This is a full-blown federal lawsuit. Honestly, this is the point where hiring an experienced attorney is practically a necessity. The court will determine if the proper legal and procedural rules were followed from the very beginning.
These higher appeal levels are often where complex cases finally get resolved. For example, a denial for a new, expensive cancer treatment might be overturned by an ALJ who gives more weight to an oncologist's testimony than the initial plan administrator did.
Navigating the appeals system is a tough road, and sometimes it makes people rethink their coverage altogether. Our guide on how to change from Medicare Advantage to Medigap can help you explore different coverage pathways that might be a better fit for your health needs down the line.
How to Appeal Medicare Advantage Denials
When you have a Medicare Advantage (Part C) plan, fighting a denial works a bit differently. These plans are run by private insurance companies, so the first few steps of an appeal are handled directly by them, not by Medicare. Getting this part right is the key to successfully turning a "no" into a "yes."
The process kicks off when your plan issues its initial denial, which is officially called an Organization Determination. This is their formal decision to refuse payment for a service or treatment. Once you get that notice, the clock starts ticking—you generally have 60 days to request their internal review, known as a Reconsideration.
This first appeal is absolutely the most critical stage of the whole process.
Navigating the Plan Reconsideration
Since you’re dealing directly with your private insurer, you need to play by their rules. Every plan has its own specific forms and procedures, so your first move should be to call the member services number on your insurance card. Ask for the exact steps and any paperwork needed to file a formal appeal. Don't just go by what the denial letter says; get confirmation over the phone.
Here’s a pro tip I always give my clients: you have the right to ask for a complete copy of your case file from the insurance plan. Do it right away. This file has everything they used to make their decision—medical records, notes from your doctor, and their own internal reviews. Seeing their reasoning lets you build a powerful counter-argument that tackles their specific points head-on.
When an Independent Review Is Needed
What if the plan stands by its denial even after your Reconsideration? Don't worry, that's not the end of the road. Your case is automatically sent for an independent, third-party review. This is where the process starts looking more like the traditional Medicare appeals system.
Your file will go to a Qualified Independent Contractor (QIC), an organization that has zero connection to your insurance company. They bring a fresh pair of eyes to your claim, looking at all the evidence from both sides to see if the denial was fair according to Medicare's rules.
If the QIC also rules against you, you can keep going. The next levels—an ALJ hearing, an Appeals Council review, and finally, Federal Court—follow the same path as appeals for Original Medicare.
One of the biggest mistakes people make is treating a Part C appeal like an Original Medicare one right from the start. The shorter deadlines and plan-specific rules in the early stages can easily trip you up. Always, always confirm the timeline with your plan and get it in writing if you can.
Thinking ahead about your health coverage can make all the difference. Proper retirement health insurance planning helps you pick a plan that truly fits your needs, which can help you avoid some of these tough denial situations in the first place.
Success Rates for Part C Appeals
Does appealing a Medicare Advantage denial actually work? The numbers say yes. It’s far from a lost cause. In fact, people are fighting back—in the second quarter of 2025 alone, beneficiaries filed 73,323 reconsideration requests.
Take a look at how often appeals are overturned for different services.
Medicare Advantage Appeal Success Rates by Service
| Service Category | Appeal Overturn Rate (Favorable) |
|---|---|
| Practitioner Services | 16.3% |
| Surgery | 15.6% |
| Inpatient Hospital | 13.5% |
| Skilled Nursing Facility | 9.7% |
| Home Health | 5.4% |
Source: Part C appeals fact sheet
As you can see, success rates vary a lot depending on what was denied. But these figures prove that a well-built appeal has a real chance of getting approved. It’s worth the effort.
Actionable Strategies for a Stronger Appeal
Navigating the Medicare appeals process successfully isn't just about following the steps—it's about smart preparation. Winning an appeal often comes down to building a strategic case that tells a compelling story, backed by solid evidence.
Think of it this way: your first move happens the moment you get that denial notice. This is when you start building your case file. Get a dedicated folder or binder and put everything in it. The initial Medicare Summary Notice, notes from phone calls, copies of letters—it all goes in. This isn't just about being tidy; it's about creating a complete, instant-access record of your journey.
Document Everything Relentlessly
You need to create a communication log. Seriously. Every single time you talk to someone from Medicare, your doctor's office, or your insurance plan, write it down.
- Who you spoke with: Get their full name and ID number if you can.
- Date and time of the call: Be as precise as possible.
- What was discussed: Jot down the key points, any advice they gave you, and any promises they made.
This log is more than just notes; it's your evidence. It can be a lifesaver if you start getting conflicting information from different people. It cuts through the frustrating "he said, she said" arguments and turns your experience into a documented, factual timeline.
A strong appeal tells a clear, consistent story. Your documentation is the backbone of that story, providing the facts needed to support your claim that a service was medically necessary and wrongly denied.
Leverage Your Doctor's Expertise
A letter of support from your doctor is probably the single most powerful tool you have. But here's the thing: a generic, one-sentence note just won't cut it. You need a detailed, evidence-based letter that directly tackles the reasons for the denial.
Ask your physician to get specific. The letter should include:
- Your diagnosis and relevant medical history.
- A clear explanation of why the denied service or item is critical for your treatment.
- The potential consequences if you don't receive this care.
- References to Medicare's own coverage guidelines, if possible, to show how the service meets their criteria.
When your doctor frames the appeal with this level of detail, it becomes much harder for reviewers to dismiss. It connects your personal health needs directly to established medical standards and the insurer's own rules. Getting familiar with common insurance claim denial reasons can also help you and your doctor anticipate their arguments and proactively strengthen your appeal.
Got Questions? We’ve Got Answers

Jumping into the Medicare appeals process can feel like a maze, and it’s completely normal to have questions pop up along the way. We’ve put together some straightforward answers to the things people ask us most often when they’re fighting a denial.
Think of this as a quick guide based on real-world situations, designed to make this whole journey a little less intimidating.
How Long Does This Whole Appeals Thing Take?
Honestly, it depends entirely on which level of the appeal you’re at. Every stage has its own federally required deadline, so the timeline can change dramatically as you move through the process.
Here’s a quick breakdown:
- Level 1 (Redetermination): The contractor handling your appeal usually has to give you an answer within 60 days of getting your request.
- Level 2 (Reconsideration): The next step is pretty similar. The QIC also generally has 60 days to make its decision.
But if you have to push your case further, things can slow down. A Level 3 hearing with an Administrative Law Judge can drag on for months—sometimes even over a year—because of major backlogs.
The one exception? If waiting for a standard decision could seriously endanger your health, you can request an expedited appeal. In those critical cases, a decision can come back in as little as 72 hours.
Can My Doctor Handle the Appeal for Me?
Yes, absolutely—and they often do! You have every right to appoint someone to act as your representative. This could be a family member, a lawyer, or your own doctor.
To make it official, you’ll just need to fill out and sign the "Appointment of Representative" form (CMS-1696). Your doctor's office can be your greatest ally here. They have all the medical records needed to build a powerful case and are usually more than willing to manage the first couple of appeal levels for you.
A great first step is to talk to the billing or administrative staff at your doctor's office. They deal with insurance denials every single day and can be an incredibly experienced partner, especially in the early stages.
What if I Messed Up and Missed a Deadline?
Missing a deadline feels like a huge setback, but don't panic. It’s not necessarily the end of the road for your appeal. If you have a legitimate reason—what Medicare calls "good cause"—for being late, you can still submit your request.
You’ll need to write down a clear explanation of why you missed the deadline and include it with your appeal. Valid reasons often include things like:
- You had a serious illness that kept you from filing on time.
- Your records were destroyed in something like a fire or flood.
- You never actually received the notice about the original denial.
The group reviewing your case will look at your reason and decide if it’s strong enough to accept your late filing.
Trying to figure out healthcare costs is tough, but you're not in it alone. Here at My Policy Quote, our goal is to help you find the right insurance to protect both your health and your finances. Take a look at your options today at https://mypolicyquote.com.


