If you don’t get health insurance through a job, you’re not alone. Individual health insurance plans are your personal safety net, bought directly from an insurance company. They’re designed for people just like you—individuals and families who need to find their own coverage.
This ensures you can handle medical bills and get the care you need, right when you need it.
Understanding Your Personal Health Coverage

Think of an individual health plan like a gym membership for your health. You pay a monthly fee—your premium—to keep your access active. But instead of just getting you in the door, this membership provides huge discounts on everything from a routine check-up to an unexpected trip to the ER.
Without it, you'd be on the hook for the full, often staggering, cost of every single medical service. With it, you share those costs with your insurance provider. This simple partnership makes healthcare predictable and affordable.
At its core, that’s what individual health insurance is all about: shielding you from a financial crisis when a medical one hits.
Who Needs an Individual Plan?
These plans are a lifeline for a huge and growing number of people who don't fit into the traditional employer-sponsored box. If any of these sound like you, an individual plan is probably your best bet:
- You're Self-Employed or a Gig Worker: Freelancers, contractors, and small business owners depend on these plans to stay protected.
- Your Employer Doesn't Offer Insurance: Many small companies or part-time jobs just don't offer health benefits.
- You're Between Jobs: An individual plan is the perfect bridge to keep you covered while you hunt for your next role.
- You're an Early Retiree: If you retire before you’re eligible for Medicare at age 65, you’ll need your own coverage.
This isn't some tiny niche market, either. It’s exploding. The global individual health insurance market was valued at around USD 654.5 million in 2024 and is expected to more than double to USD 1,398.8 million by 2032. This massive growth shows just how many people are realizing the need for personal health coverage. You can dig into these trends in the full report from Fortune Business Insights.
A lot of people think buying insurance on your own is impossibly complicated. The truth is, it just comes down to understanding a few key ideas. Once you get the basics of how these plans work, you can confidently pick one that fits your health needs and your budget.
Ultimately, getting an individual health plan is a powerful move for your financial stability and your peace of mind. It gives you the freedom to get preventive care, manage chronic conditions, and handle emergencies without putting your future at risk.
Next, we'll break down the different types of plans out there, so you can see which "membership" style is the right fit for you.
Decoding the Different Types of Health Plans
When you start looking for an individual health insurance plan, you’ll immediately see a few acronyms pop up: HMO, PPO, and EPO. They aren’t just random letters—they’re the blueprints for how you’ll get and pay for your medical care.
Figuring out the difference between them is the single most important step in finding a plan that actually fits your life.
Think of it like choosing a metro card for a new city. One pass might be cheap but only works on a specific subway line. Another might let you ride buses, trains, and even ferries, giving you total freedom for a higher price. Health plans work the same way, balancing the size of the doctor network, your costs, and your freedom to choose.
The three main plan types you’ll run into are HMOs, PPOs, and EPOs.
The image below shows how these plans are all different branches of the same tree—individual health coverage.
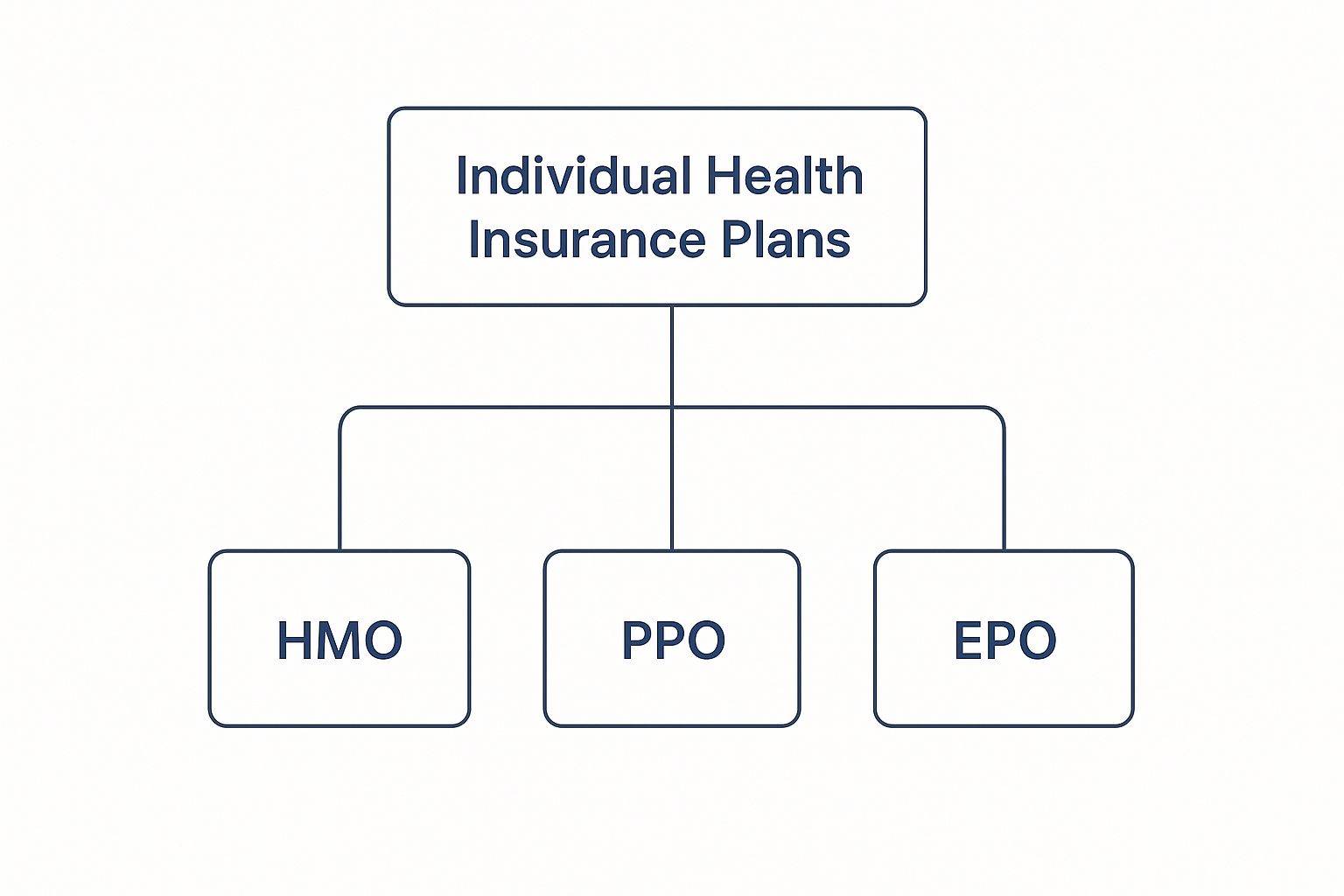
While they all fall under the same umbrella, the rules for how they operate are what set them apart.
HMO: Health Maintenance Organization
An HMO, or Health Maintenance Organization, is like that closed-loop subway system. It runs on a specific network of doctors, hospitals, and specialists who’ve all agreed to provide care at a lower cost for members.
To make that work, an HMO requires you to stay within its network to be covered. The only exception? A true emergency.
The defining feature of an HMO is your Primary Care Physician (PCP). This is your go-to doctor, the person who acts as your home base for all things health-related. If you need to see a specialist, like a cardiologist or an allergist, you have to get a referral from your PCP first. This keeps your care coordinated and helps keep costs down.
HMOs are often the most affordable plans you can find. If you’re okay with a structured system and getting referrals for specialized care, an HMO can be a fantastic, budget-friendly choice.
But remember, the structure is strict. If you see a doctor outside the approved network without permission, you’ll likely have to pay 100% of the bill yourself.
PPO: Preferred Provider Organization
A PPO, or Preferred Provider Organization, is that all-access pass we talked about. It offers way more flexibility. You have a "preferred" network of providers where your costs are lowest, but you also have the freedom to go "off-network" to see any licensed doctor you want.
That freedom comes at a price. Your out-of-pocket costs—like copayments and coinsurance—will be a lot higher when you see an out-of-network provider. PPOs also tend to have higher monthly premiums than HMOs.
A huge perk is that you do not need a referral from a PCP to see a specialist. You can just book the appointment yourself.
This freedom makes PPOs a great fit for people who:
- Want to go directly to specialists without waiting for a referral.
- Travel often and might need medical care in different parts of the country.
- Already have a doctor they love and want to keep seeing, even if that doctor isn't in-network.
EPO: Exclusive Provider Organization
An EPO, or Exclusive Provider Organization, is a blend of an HMO and a PPO. Like an HMO, it requires you to use doctors and hospitals within its network for your care to be covered. There’s typically no coverage for out-of-network care unless it’s an emergency.
But, like a PPO, an EPO does not require you to have a PCP or get referrals to see specialists. This gives you the direct-access feel of a PPO but with the lower costs that come from a more contained network. EPO networks are often larger than HMO networks, giving you more choices while still keeping costs in check.
To make things even clearer, here’s a quick rundown of how the big three stack up against each other.
HMO vs PPO vs EPO At a Glance
| Feature | HMO (Health Maintenance Organization) | PPO (Preferred Provider Organization) | EPO (Exclusive Provider Organization) |
|---|---|---|---|
| Primary Care Physician (PCP) | Required. Your PCP manages your care. | Not Required. You can manage your own care. | Not Required. You can manage your own care. |
| Referrals for Specialists | Required for most specialist visits. | Not Required. You can see specialists directly. | Not Required. You can see specialists directly. |
| Out-of-Network Coverage | No coverage, except for emergencies. | Yes, but at a higher out-of-pocket cost. | No coverage, except for emergencies. |
| Overall Cost | Typically lower premiums and out-of-pocket costs. | Typically higher premiums and out-of-pocket costs. | A middle ground between HMO and PPO costs. |
| Best For | People who want lower costs and coordinated care. | People who want maximum flexibility and choice. | People who want direct access to specialists at a lower cost. |
Choosing the right plan isn't just about the monthly premium; it's about matching the plan's structure to your own health needs and lifestyle.
As you navigate traditional insurance, remember there are other models out there, too. Some people find that clinic-specific membership plans as alternative healthcare coverage can be a different way to manage costs. To get the full picture, take a look at our guide comparing individual vs. group health insurance. It’ll help you understand all the options on the table.
Making Sense of Your Health Insurance Costs

To really get a feel for a health insurance plan, you have to look beyond the monthly price tag. That number is important, sure, but it’s just one piece of a much bigger financial puzzle. The true cost of your plan only reveals itself when you actually need to use it.
Think of it like this: your plan is a shared "healthcare piggy bank." Every cost you see is just a different rule for how money goes into and comes out of that bank.
Once you understand these rules, you can pick a plan that protects both your health and your wallet. Let's break down the four key terms you’ll see everywhere: premium, deductible, copayment, and coinsurance.
Your Premium: The Monthly Entry Fee
The premium is the most straightforward cost. It's the fixed amount you pay every month to keep your insurance active, whether you see a doctor or not.
It’s like the automatic deposit you make into that shared piggy bank. This payment keeps your plan ready to go the moment you need it.
If you miss these payments, your coverage can lapse, leaving you completely unprotected. This is the foundational cost you absolutely must budget for.
The Deductible: Your Initial Contribution
The deductible is how much you have to pay out-of-pocket for medical care before your insurance company starts chipping in. For example, if your plan has a $3,000 deductible, you’re on the hook for the first $3,000 of your medical bills for the year.
It’s the amount you have to fill the piggy bank with yourself before your insurer starts making its own deposits. Once you hit that number, the cost-sharing really begins.
Your deductible resets every year. It’s a crucial number because a plan with a low monthly premium might come with a sky-high deductible, meaning you'll pay a lot more upfront when you need care.
This is a classic trade-off. For more on how to balance these costs, check out our guide on finding affordable health insurance with quality coverage.
Copayments and Coinsurance: Sharing the Bill
Once you’ve met your deductible, you don’t stop paying completely. Instead, you start sharing the bill with your insurance company. This happens in two main ways.
- Copayment (Copay): This is a simple, flat fee you pay for a specific service. You might have a $30 copay for a regular doctor’s visit or a $50 copay to see a specialist. It’s a predictable cost for routine care.
- Coinsurance: This is a percentage you pay after meeting your deductible. If your plan has 20% coinsurance and a hospital stay costs $10,000, you’d be responsible for $2,000.
Think of a copay like a small, set toll for using a service. Coinsurance is more like agreeing to pay a percentage of the total construction cost of the road you just drove on.
The Out-of-Pocket Maximum: Your Ultimate Financial Shield
Finally, every plan has an out-of-pocket maximum. This is the absolute most you will have to pay for covered medical care in a single year. This number includes your deductible, copays, and coinsurance payments.
Once you hit this limit, your insurance plan pays 100% of the costs for covered services for the rest of the year. It’s your ultimate financial safety net, protecting you from crippling costs if a major illness or injury occurs.
Understanding this cap is vital. It represents your total financial exposure for the year and gives you true peace of mind.
How and When You Can Enroll in a Plan
Unlike most things you buy, you can’t just sign up for a health insurance plan whenever you feel like it. The system is built around specific windows of time, and knowing when they are is the key to getting covered without a headache.
There are two main ways to enroll: the annual Open Enrollment Period and a Special Enrollment Period.
Think of Open Enrollment as the main event for everyone. A Special Enrollment Period, on the other hand, is a private opportunity that opens up only after a major life change.
This structure is there for a reason. The global health insurance market is massive—projected to hit nearly USD 5.12 trillion by 2034. With sky-high healthcare costs and about 60% of Americans living with a chronic condition, the demand is huge. You can get a closer look at these trends in this global health insurance market outlook.
The Annual Open Enrollment Period
The Open Enrollment Period (OEP) is the one time of year when pretty much anyone can buy, switch, or renew their individual health plan for the year ahead.
It usually runs from November 1 to January 15 in most states. Some states that run their own marketplaces might have slightly different dates, so it's always good to double-check.
This is your official window to shop around, compare new plans, and make sure your current one still makes sense for you. If you miss it and don't have a qualifying life event, you could be stuck waiting a whole year for your next shot at coverage.
Think of Open Enrollment as the yearly "health check" for your insurance plan. It's the perfect time to ensure your coverage aligns with your budget, health needs, and doctor preferences for the year ahead.
Seriously, mark these dates on your calendar. For a deeper dive, check out our guide that explains what Open Enrollment is and why it matters.
Unlocking a Special Enrollment Period
But what if you need insurance outside of that annual window? That’s what a Special Enrollment Period (SEP) is for.
An SEP is a 60-day window to sign up for a new plan that opens up after you experience a “qualifying life event.” These are big life changes that can shake up your healthcare needs or your ability to get coverage. It's the system’s way of making sure you’re not left uninsured because of things outside your control.
So, what counts as a qualifying event? The most common ones include:
- Losing Other Health Coverage: Maybe you left a job, got divorced from the person whose plan you were on, or you’re turning 26 and aging off a parent’s plan.
- Changes in Your Household: Big family changes like getting married, having a baby, or adopting a child will all open an SEP for you.
- Moving to a New Area: If you move to a new ZIP code or county where your current plan isn't available, you get a chance to enroll in a new one.
- Changes in Your Income: If your household income changes enough, you might suddenly qualify for subsidies that help lower your monthly premium.
These events act like a special key, temporarily unlocking the door so you can get the coverage you need, right when you need it.
Choosing the Right Health Plan for Your Life

Alright, you’ve got the basics down on plan types and how the costs work. Now it’s time to put that knowledge into action and make a decision you can feel good about.
Choosing from all the individual health insurance plans out there isn't about finding some magical "best" option. It's about finding the one that’s best for you.
This takes a little honest self-reflection—think of it as a personal health audit. By looking at your typical medical needs, your budget, and what you value most in a plan, you can cut through the noise and find a perfect match for your life.
Start With a Personal Health Audit
Before you even glance at a single plan, take a moment to ask yourself a few key questions. Getting this part right is the foundation for a smart choice you won't regret down the road.
Grab a notebook and jot down your answers:
- How often do you really see a doctor? Are you generally healthy and just go for an annual check-up, or do you have a chronic condition that needs regular attention?
- Do you take any prescription drugs? List out any medications you take consistently. You'll need to make sure they’re on a plan’s formulary (its list of covered drugs).
- Is it important to keep your current doctors? If you have a primary care physician or a specialist you trust, you’ll want to check if they are in-network. This is a deal-breaker for many people.
- Are you planning any major medical events? Think about anything on the horizon, like starting a family, a planned surgery, or managing a new diagnosis.
Answering these questions gives you a personalized filter. It lets you immediately cross off plans that don't cover your prescriptions or include your doctor, saving you a ton of time and frustration.
For those navigating this on their own as a freelancer or small business owner, we have a guide that digs deeper into the best health insurance for the self-employed.
Understanding the Metal Tiers
When you shop for a plan on the Health Insurance Marketplace, you’ll see them grouped into four "metal" tiers: Bronze, Silver, Gold, and Platinum.
Don't let the names fool you—this has nothing to do with the quality of care you receive. It's just a simple way to show how you and your insurance company will split the costs.
Think of it like a cell phone plan. A cheap plan might have a low monthly fee but charge you a fortune if you go over your data limit. A pricier one might have a high monthly fee but offer unlimited data, so you never get a surprise bill. The metal tiers work the same way for healthcare costs.
Here’s the simple breakdown:
- Bronze: You pay the lowest monthly premium, but your out-of-pocket costs will be the highest when you need care. Your deductible could be thousands of dollars. This is often a good fit for healthy people who just want a safety net for worst-case scenarios.
- Silver: This is the happy medium, with moderate premiums and moderate costs for care. Crucially, Silver is the only tier where you might qualify for Cost-Sharing Reductions (CSRs)—extra subsidies that lower your deductible and copays.
- Gold: You'll pay a higher monthly premium, but your plan covers more of your medical bills. Deductibles are much lower, making this a solid choice if you expect to need regular medical care.
- Platinum: This tier has the highest monthly premium, but it also pays the most toward your care. Deductibles are very low or even $0, which makes your healthcare costs extremely predictable.
The key is to balance what you pay each month with what you might have to pay when you actually use your insurance. A low-premium Bronze plan looks great at first, but one unexpected trip to the ER could leave you with a massive bill.
Making Your Final Decision
Once your health audit is done and you know which metal tier feels right, you’re ready to compare your final options. For every plan you’re considering, look for the Summary of Benefits and Coverage. It’s a standardized document that makes it easy to compare costs and coverage side-by-side.
Focus on the total financial picture, not just the monthly premium. A Gold plan with a higher premium might actually save you money over the year compared to a Bronze plan if you know you’ll hit that high deductible anyway.
Ultimately, the right choice is the one that gives you peace of mind. It should connect you with the doctors you trust and protect your savings from a medical emergency—all within a budget you can handle.
Burning Questions About Individual Health Insurance
Even after you get the basics down, a few nagging questions always seem to pop up when you're comparing individual health insurance plans. Getting straight answers is the last step before you can feel truly good about your decision.
Think of this as your final walkthrough. You’ve seen the major features, but now it’s time to ask those last few critical questions before you sign. Let's clear up any remaining confusion.
Can I Be Denied for a Pre-existing Condition?
This is a huge source of stress for people buying their own insurance, and the answer is a firm no. Thanks to the Affordable Care Act (ACA), insurance companies can't legally turn you away or charge you more just because you have a pre-existing condition.
This is one of the most important protections in modern health insurance. It means things like diabetes, asthma, or even a past injury can't be held against you when you apply for an ACA-compliant plan.
Before the ACA, insurers could dig through your medical history and either refuse to cover you or exclude treatments for your condition. Today, that’s no longer a worry with compliant plans, ensuring everyone has a fair shot at getting care.
This rule applies to every plan on the Health Insurance Marketplace and most plans sold directly by insurers. It’s huge for peace of mind, knowing your health history won’t lock you out of coverage.
What Is the Difference Between ACA Plans and Short-Term Plans?
This is a really important distinction. While both are types of individual insurance, they're built for completely different situations and offer wildly different levels of protection.
An ACA plan is like a comprehensive homeowner's policy. It's designed to cover you for everything from a small leak to a catastrophic fire. A short-term plan is more like temporary insurance for a weekend rental car—it covers a few specific risks for a very brief time and has massive gaps.
Here’s a simple breakdown:
- ACA-Compliant Plans: These are the plans you find on the Marketplace. They are required to cover 10 essential health benefits, like hospital stays, prescriptions, and maternity care. They also guarantee coverage for pre-existing conditions.
- Short-Term Health Insurance: These plans are just temporary fixes, maybe for a month or two between jobs. They are not required to cover essential benefits and they can and do deny coverage for pre-existing conditions. Their coverage is very limited, and they often cap how much they’ll pay.
Short-term plans might look tempting with their low monthly premiums, but they are absolutely not a substitute for a real ACA plan. They’re a band-aid, not a safety net.
How Do I Know if I Qualify for a Subsidy?
A lot of people are shocked to find out they qualify for financial help that makes their insurance plan much more affordable. These subsidies, or tax credits, are there to lower your monthly premium and sometimes your out-of-pocket costs, too.
Your eligibility is mostly based on your household size and your Modified Adjusted Gross Income (MAGI). You don't have to have a low income to qualify—many middle-class families and individuals get significant help. For 2025, a single person making up to $60,240 or a family of four earning up to $124,800 could get a premium tax credit.
There are two kinds of subsidies you can get through the Marketplace:
- Premium Tax Credits (PTCs): This is the main one. It directly lowers your monthly premium. You can have it sent straight to your insurer each month or get it all back when you file your taxes.
- Cost-Sharing Reductions (CSRs): This is extra help for people with lower incomes. If you qualify, CSRs lower your out-of-pocket costs like your deductible and copays when you choose a Silver-level plan.
The only way to know for sure is to fill out an application on the Health Insurance Marketplace. The system does the math for you and shows you exactly how much you can save on different individual health insurance plans.
Figuring out your health coverage options can feel complicated, but you don’t have to do it alone. The experts at My Policy Quote are here to help you understand your choices and find a plan that fits your life and your budget. Explore your personalized options and get a free quote today at mypolicyquote.com.