Think of your health insurance deductible as the amount you have to pay for your medical care before your insurance company starts chipping in. It’s your share of the deal, the initial hurdle you clear each year.
Once you’ve paid that specific amount out-of-pocket for covered services, your plan’s real benefits kick into high gear.
How a Health Insurance Deductible Actually Works
Let's make this simple. Imagine your deductible is like the entry fee to an all-inclusive resort. You have to pay that one-time fee to get your wristband. Before you do, you're on your own for everything. But once you've paid it, you unlock all the resort’s benefits.
It’s the same with health insurance. You cover your medical bills until you hit that deductible number.
After you've met that threshold, you’re not flying solo anymore. You enter a cost-sharing phase with your insurer. This is where terms like copayments and coinsurance come into the picture, and you start paying just a piece of the bill instead of the whole thing.
The Annual Reset Button
Here’s a detail you can’t forget: your deductible resets every year. For the vast majority of plans, this happens on January 1st.
That means even if you hit your deductible in December after a big medical expense, the counter goes back to zero as soon as the new year begins. You have to meet that "entry fee" all over again to unlock your plan's cost-sharing benefits for the new year.
Your deductible is the gatekeeper to your health plan's best features. Once you meet it, you open the door to more affordable care for the rest of the year.
This concept is especially important for different groups to understand. For seniors navigating their options, for example, grasping how deductibles work within different programs is essential. You can learn more about how this plays out in programs like Medicare and Medicaid in Ohio Senior Care.
To see this in action, let’s break down how your costs change.
Your Costs Before vs After Meeting Your Deductible
This table gives you a clear snapshot of how your payment responsibility shifts once you've satisfied your deductible for the year.
| Scenario | Your Responsibility (What You Pay) | Insurance Company's Responsibility (What They Pay) |
|---|---|---|
| Before Meeting Deductible | You pay 100% of the allowed cost for most services. | The insurance company pays $0 (outside of certain preventive care). |
| After Meeting Deductible | You pay just a portion of the costs (your copay or coinsurance). | The insurance company pays the majority of the costs. |
Getting a handle on this "before and after" is the key to planning your healthcare spending. Some plans even have a feature where there is https://mypolicyquote.com/2025/09/11/what-does-no-charge-after-deductible-mean/ for certain services, which is a game-changer for your budget once you've hit that initial mark.
Navigating Your Total Out-of-Pocket Costs
Understanding your deductible in health insurance is a great start, but it’s just one piece of the puzzle. To really get a grip on your total healthcare spending, you need to see how the deductible, premium, copayments, and coinsurance all lead up to your ultimate safety net: the out-of-pocket maximum.
Let's walk through a real-world example to connect the dots. Meet Sarah, a freelance graphic designer whose health plan has a $3,000 deductible and an $8,000 out-of-pocket maximum.
The Starting Point: Your Monthly Premium
Before any doctor's visits even happen, Sarah pays her monthly premium. This is the fixed amount she pays every month just to keep her insurance active.
Think of it like a subscription—it doesn’t count toward her deductible, but it guarantees her coverage is ready and waiting when she needs it. It’s a predictable cost that’s totally separate from what she pays for actual medical care.
Phase 1: Meeting the Deductible
Early in the year, Sarah comes down with a nasty flu and heads to an urgent care clinic. The total allowed cost for the visit and her prescription comes to $250. Since she hasn't paid anything toward her deductible yet, she covers the full $250 herself.
Now, her remaining deductible is down to $2,750 ($3,000 – $250).
A few months later, she has a minor accident and needs imaging at a hospital. The bill is $2,800. She pays the remaining $2,750 of her deductible, and just like that, she has officially met her $3,000 deductible for the year. The simple visual below shows this journey from paying initial costs to reaching the next phase.
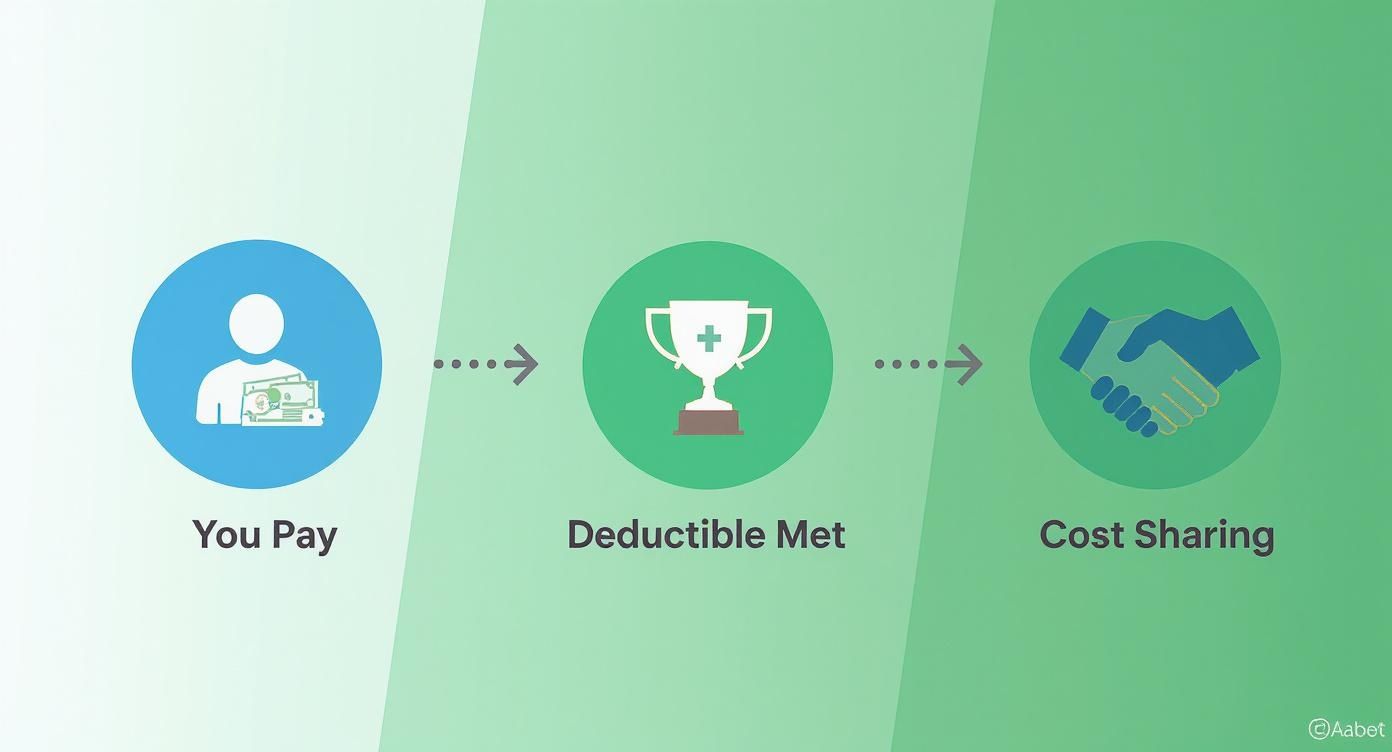
This flow is the key: you cover costs yourself until the deductible is met, which unlocks the cost-sharing power of your plan.
Phase 2: The Cost-Sharing Stage
With her deductible now satisfied, Sarah’s insurance plan really kicks into gear. She’s now in the cost-sharing phase, which means she no longer has to pay 100% of the bill for covered services.
Her plan has 20% coinsurance. This means for any new medical expense, her insurance pays 80% of the cost, and she's responsible for the other 20%. This teamwork continues until she hits her final spending limit. Getting the difference between these payment types is crucial, and you can get a deeper look in our guide on coinsurance vs copay.
Phase 3: Reaching the Out-of-Pocket Maximum
Later in the year, Sarah needs an unexpected outpatient surgery. The total cost is a staggering $30,000.
Since her deductible is already met, she only owes her 20% coinsurance. Twenty percent of $30,000 is $6,000. But wait—her plan has an $8,000 out-of-pocket maximum. She’s already paid $3,000 for her deductible, so she only needs to pay $5,000 more before she hits that ceiling.
The out-of-pocket maximum is your financial shield. It is the absolute most you will have to pay for covered medical services in a single year.
So, for that $30,000 surgery, Sarah pays $5,000. This brings her total spending for the year (deductible + coinsurance) to exactly $8,000.
What happens now? For the rest of the year, her insurance company will pay 100% of all her covered medical costs. She won’t owe another dime in copays or coinsurance until her plan resets on January 1st. This progression—from premium to deductible to cost-sharing and finally to the out-of-pocket max—is the complete financial journey of a health insurance plan.
Individual vs Family Deductibles
When you're covering more than just yourself, the idea of a deductible in health insurance gets a little more interesting. Family plans aren’t as simple as having one single deductible. They usually come in two flavors, and the difference can totally change when—and how—your insurance starts to pay.
Getting this right isn't just a minor detail. It's the key to managing your family's healthcare budget without nasty surprises. Choosing the right structure can be the difference between getting financial help early in the year or having to wait until several family members rack up big medical bills. For a bigger picture, our guide on individual and family health plans offers more context.

The Embedded Deductible Explained
Most family plans today use an embedded deductible. Think of it as a two-level system: each person on the plan gets their own individual deductible, which is "embedded" inside a larger, overall family deductible.
Here’s why that’s so helpful: once any single person meets their individual deductible, the insurance company starts paying its share for that person's medical bills. They don’t have to wait for the entire family to hit the bigger number. This is a huge relief if one family member has a major health event early in the year.
For instance, say your plan has a $3,000 individual deductible and an $8,000 family deductible. If your child needs a $4,000 surgery, your insurance kicks in after you've paid the first $3,000. Relief comes much sooner.
The Aggregate Deductible Explained
An aggregate deductible is a whole different ballgame. With this setup, there's just one, single bucket of a deductible for the entire family. Every medical expense from every person on the plan gets thrown into this one big pot.
With an aggregate deductible, no cost-sharing help kicks in for anyone until that one massive family deductible is met. This can lead to some serious out-of-pocket costs at the start of the year, especially if medical needs are spread out across the family instead of being focused on one person.
An embedded deductible offers individual safety nets within the larger family plan, while an aggregate deductible requires the entire family to work together to meet one combined financial threshold.
Imagine a plan with a $10,000 aggregate deductible. If three different family members each have $3,000 in medical costs, that’s $9,000 you’ve spent. But you would have to pay every single dollar of it yourself because you still haven't hit the $10,000 magic number for the insurance to start helping.
Embedded vs Aggregate Deductibles: A Family Plan Comparison
Let's put some real numbers to this to see how it plays out for a family of four. Imagine they're choosing between two plans that, on the surface, look very similar.
| Scenario | Embedded Deductible Plan | Aggregate Deductible Plan |
|---|---|---|
| Plan Details | $3,000 individual deductible, $8,000 family deductible | $8,000 family deductible |
| The Event | One family member, Alex, has a hospital stay costing $5,000. | One family member, Alex, has a hospital stay costing $5,000. |
| How It's Paid | The family pays $3,000 to meet Alex's individual deductible. The insurance company starts paying its share on the remaining $2,000 (minus coinsurance). | The family pays the full $5,000 bill out of pocket. The insurance company pays nothing yet, as $3,000 is still left on the family deductible. |
| The Result | Immediate financial relief. The other family members still have their own deductibles to meet, but Alex is now covered. | The family is out $5,000 and is still a long way from getting any help from their insurance plan. |
As you can see, the embedded plan provides a critical safety net when one person has a significant medical need. While both plans have the same total family deductible, the way you get there makes all the difference in your out-of-pocket spending. The choice between these two structures can have a massive impact on your family’s finances.
Using an HSA with a High Deductible Health Plan
A plan with a higher deductible in health insurance might sound a bit intimidating at first. More risk, right? But here's the thing: it often unlocks one of the most powerful financial tools out there for healthcare—the Health Savings Account (HSA).
When you pair a High-Deductible Health Plan (HDHP) with an HSA, you're not just paying for insurance anymore. You’re actively building a tax-advantaged savings fund for your health.

This combo is a deliberate strategy. HDHPs usually have much lower monthly premiums, which frees up cash. Instead of just giving that money to the insurance company, you can redirect it straight into your HSA, giving you full control over how your healthcare dollars are spent and saved.
What Qualifies as an HDHP
Hold on, though—not just any plan with a high deductible counts. To be "HSA-eligible," a plan has to meet specific IRS rules. Each year, the government sets minimum deductible amounts and maximum out-of-pocket limits that a plan must fall within to officially be considered an HDHP.
To open and contribute to an HSA, you need to be enrolled in one of these qualifying plans. You also can't be covered by another non-HDHP plan, enrolled in Medicare, or claimed as a dependent on someone else's taxes. The rules are specific, but getting through that checklist opens the door to some serious financial perks.
The Triple Tax Advantage of an HSA
There's a reason people in the know get excited about HSAs. It’s often called the ultimate retirement account, and that's thanks to its unique triple tax advantage. No other savings account can touch this.
- Tax-Deductible Contributions: The money you put into your HSA lowers your taxable income for the year. Simple as that.
- Tax-Free Growth: If you choose to invest your HSA funds, any earnings they generate grow completely tax-free.
- Tax-Free Withdrawals: You can pull money out for qualified medical expenses anytime without paying a single penny in taxes.
This triple-threat benefit makes an HSA more than just a piggy bank for doctor's visits; it’s a powerful investment vehicle. And the best part? The money is yours. It rolls over year after year, continuing to grow.
An HSA is like a 401(k) for your health, but better. It gives you tax breaks on the way in, while it grows, and on the way out for medical needs.
How an HSA Becomes a Retirement Fund
While your HSA is perfect for covering today's costs like prescriptions, dental work, and specialist visits, its real magic happens over the long haul. Many savvy savers use it as a stealth retirement account.
Here's how: once you turn 65, you can withdraw money from your HSA for any reason—not just medical bills—without that stiff 20% penalty. For non-medical expenses, you'll just pay regular income tax on the withdrawal, exactly like you would with a traditional 401(k) or IRA.
This flexibility is a game-changer. By paying for smaller medical costs out-of-pocket now and letting your HSA grow untouched, you can build a substantial nest egg for your future. Whether you use it for healthcare in retirement or to fund your dreams, the choice is yours.
The list of what you can use it for is surprisingly long, covering everything from acupuncture to prescriptions. To get a better feel for it, it’s helpful to see what can you use your HSA for in our detailed guide.
Choosing the Right Deductible for Your Life
There’s no magic number for the perfect deductible in health insurance. The best choice is deeply personal and really comes down to balancing what you can afford each month with what you could handle if a big medical bill showed up.
Think of it like a seesaw. A lower monthly premium usually means you’re taking on a higher deductible. On the flip side, a higher premium often gets you a lower one.
Finding that sweet spot means being honest about your health, your savings, and how much risk you’re comfortable with. So, instead of generic advice, let’s walk through what this looks like for real people in different stages of life.
For the Young and Healthy Professional
If you’re young, in great health, and your doctor visits are mostly for annual checkups, a high-deductible health plan (HDHP) can be a really smart move. Your main goal is keeping your monthly bills low while still having a safety net for a real emergency.
The lower premium frees up cash every month. You can then sock that extra money away, maybe in a Health Savings Account (HSA), to build up a fund for that day you actually need to cover your deductible.
- The Upside: You get much lower monthly payments and can contribute to a powerful, tax-advantaged HSA.
- The Downside: An unexpected accident or illness could leave you with a big, sudden bill before your insurance kicks in.
This strategy definitely requires some financial discipline. You have to be committed to saving the money you’re not spending on premiums, just in case.
For the Growing Family
With young kids, the medical costs can feel constant—ear infections, sports physicals, and the occasional trip to urgent care for a sprained ankle. For families, predictability is everything.
A low-deductible plan might have a higher monthly premium, but it offers incredible peace of mind and makes budgeting way more stable. You’ll hit your deductible faster, which means your insurance starts sharing the costs sooner in the year.
For families, a lower deductible acts as a buffer against all those frequent but smaller medical expenses, making healthcare costs feel much more manageable from month to month.
It's a trade-off many parents are happy to make, choosing immediate access to benefits over lower fixed costs.
For the Self-Employed Freelancer
When you're a freelancer or 1099 contractor, your income can swing up and down. A high monthly premium can feel like a real burden during a slow month, which is why a high-deductible health plan often just fits better.
That lower premium gives you critical breathing room in your budget. Plus, as a self-employed person, you can often deduct your health insurance premiums from your taxes, which helps. The trick is to pair that HDHP with a dedicated savings plan, like an HSA, to build your own health fund.
This isn’t just a freelancer issue, either. Across the U.S., deductibles in employer plans have been climbing. A recent analysis shows the average deductible for a single person is now $1,886 in 2025, and a staggering 87% of workers have to meet a deductible before their plan helps with most services. You can get the full scoop on this trend in the KFF survey.
For Pre-Retirement Adults
As you get closer to retirement, your health needs can change. You might be managing a chronic condition or just find yourself needing more regular screenings and specialist visits.
At this stage, a low-deductible plan can be a very wise investment. You’re paying a higher premium, sure, but it’s a calculated expense that buys you predictable access to care when you need it. It helps ensure a large medical bill doesn’t throw a wrench in your retirement savings.
- Low Deductible: This gives you financial security and makes it easier to get care because the upfront cost barrier is much smaller.
- High Deductible: This could be a huge financial risk if you have ongoing health issues or will be on a fixed income.
Ultimately, picking the right deductible in health insurance is about matching the plan to your reality. When you weigh your health, your savings, and your comfort with risk, you can find a plan that protects both your well-being and your wallet.
Common Questions About Health Insurance Deductibles
Even when you think you have a handle on the basics, health insurance can still feel like a maze. Weird rules and specific situations pop up, leaving you scratching your head. This is where we tackle those lingering questions head-on, giving you clear, direct answers about the deductible in health insurance.
Think of this as your personal guide for all those "what if" moments. We'll clear up the confusion around everything from preventive care to changing plans mid-year, so you can walk away feeling confident about your coverage.
Does Preventive Care Count Toward My Deductible?
This is a big one, and the answer is usually a huge relief. Thanks to the Affordable Care Act (ACA), most health plans have to cover a whole list of preventive services at 100%, even if you haven't touched your deductible.
That means you can go for your annual physical, get that flu shot, or have certain health screenings without paying a dime out-of-pocket. These services are all about keeping you healthy in the first place, so they play by a different set of rules.
But here’s a crucial catch you need to know:
- Preventive vs. Diagnostic: Let's say during your "free" annual checkup, your doctor finds something that needs a closer look. Any follow-up tests or treatments are now considered diagnostic, not preventive. That diagnostic care will count toward your deductible and you'll start paying your share.
So, the initial check-in is covered, but anything done to investigate a problem is what starts chipping away at your deductible.
What Happens If I Switch Plans Mid-Year?
Life happens. Maybe you land a new job, move across the country, or have another big life event that lets you change your health plan before the year is over. The biggest worry people have is whether all the money they’ve paid toward their deductible just vanishes.
Unfortunately, most of the time, it does. When you switch to a new insurance plan—even if it's with the same company—your deductible and out-of-pocket maximum usually reset to zero. The new plan is a totally new contract, and your progress from the old one doesn't get to come along for the ride.
Key Takeaway: If you’re changing your insurance mid-year, be ready to start from square one with your deductible. It’s a huge factor to weigh when you're looking at the true cost of a new plan.
This makes it incredibly important to time any big medical procedures if you know a change is on the horizon.
Do I Have a Separate Deductible for Prescriptions?
This is a super common point of confusion because it really depends on your specific plan. Some plans lump everything together with one big deductible for both medical care and prescriptions. Others split them up.
Here’s how to figure out what you have:
- Combined Deductible: All your eligible costs—doctor visits, hospital bills, and prescription refills—count toward a single deductible. Simple.
- Separate Deductibles: You might have one deductible for medical services and a completely different one for your medications. In this case, what you spend on doctor visits won't help you meet your drug deductible, and vice versa.
You have to check your plan's "Summary of Benefits and Coverage" to know for sure. This little detail can make a massive difference in your yearly costs, especially if you rely on regular medications.
Can I Negotiate Medical Bills Before Meeting My Deductible?
Yes! Absolutely. This is one of the most powerful and underused ways to control your healthcare costs. Before you meet your deductible, you’re basically a "cash-pay" patient, and that actually gives you some power.
Many doctors and hospitals are willing to offer a discount if you can pay in full upfront. Why? It saves them the headache of billing insurance and waiting to get paid. Don't ever be afraid to ask for the "self-pay rate," which can be way lower than what they'd bill your insurance.
You can also:
- Ask for an itemized bill: Go through it with a fine-tooth comb to check for errors or services you never actually received.
- Inquire about payment plans: Most places will offer interest-free payment plans to help you break up a large bill into manageable chunks.
It never hurts to ask. The worst they can do is say no, but you'd be surprised how often they're willing to work with you. A little bit of proactive negotiation can save you hundreds, or even thousands, as you work toward meeting your deductible in health insurance.
Navigating health insurance can feel complex, but you don't have to do it alone. At My Policy Quote, we specialize in helping people find clear, affordable plans that match their life and budget. If you're ready to find coverage that truly works for you, explore your options with us today at https://mypolicyquote.com.